Gallbladder pain often starts as a dull ache after meals and slowly turns into something harder to ignore. Many people live with symptoms for months before they realise gallstones could be the cause. By the time they search for help, the real question is no longer what is wrong, but whether surgery is now unavoidable.
This matters because gallbladder conditions sit in a grey area. Some people improve with simple measures. Others delay treatment and end up in A&E with infection or pancreatitis. Knowing when to watch, when to investigate, and when to operate can prevent long-term complications and unnecessary anxiety.
This guide explains gallstones symptoms, the difference between gallstones and gallbladder inflammation, when gallbladder surgery in the UK is recommended, and what treatment pathways look like on the NHS and privately. It is written to help you make informed decisions, not to push you toward an operation.
What Causes Gallbladder Pain?
Gallbladder pain occurs when bile cannot flow freely from the gallbladder into the digestive system. In most cases, this is due to gallstones blocking the cystic duct. The gallbladder contracts after eating, particularly fatty meals, which explains why symptoms often follow food intake.
Pain may come and go, or it may progress to constant discomfort if inflammation develops. Understanding the underlying cause helps determine whether treatment can remain conservative or whether surgery is the safer option.
Gallstones vs Gallbladder Inflammation: Key Differences
Gallstones are solid crystals formed from cholesterol or pigment in bile. Many people have gallstones incidentally discovered on scans and never develop symptoms.
Typical Gallstones Symptoms
- Pain under the right ribs, often after fatty meals
- Pain radiating to the back or right shoulder blade
- Nausea or vomiting
- Episodes lasting 30 minutes to several hours
Gallbladder inflammation, known as cholecystitis, develops when blockage persists and the gallbladder becomes swollen and infected.
Red Flags Suggesting Inflammation
- Constant pain lasting more than 6 hours
- Fever or chills
- Increasing tenderness under the right ribs
- Raised inflammatory markers on blood tests
This distinction is crucial. Simple biliary colic may be managed conservatively, but confirmed inflammation usually leads to surgery.
When Conservative Gallbladder Pain Treatment Is Appropriate
Not every patient with gallstones needs an operation. Conservative management may be suitable when:
- Pain episodes are infrequent
- Symptoms are mild and short-lived
- There are no signs of infection or bile duct obstruction
- Imaging shows uncomplicated gallstones
Management focuses on dietary modification, particularly reducing fatty foods, along with pain relief during attacks. Some patients remain stable for years.
However, gallstones do not dissolve on their own. Recurrent attacks increase the risk of complications, which is why ongoing symptoms are usually reassessed.
When Is Gallbladder Surgery Recommended?
Gallbladder surgery in the UK is recommended when symptoms affect quality of life or when complications develop. Common indications include:
- Recurrent biliary colic despite lifestyle changes
- Acute cholecystitis
- Gallstone pancreatitis
- Stones migrating into the bile duct
- Thickened gallbladder wall or surrounding fluid on imaging
At this stage, surgery is considered preventative as well as curative. Delaying intervention may increase operative difficulty and risk.
Understanding Imaging and Test Results
Ultrasound Findings
Ultrasound is the first-line investigation for gallbladder problems. Clinicians assess:
- Number and size of gallstones
- Gallbladder wall thickness
- Presence of fluid around the gallbladder
- Diameter of bile ducts
Blood Test Interpretation
Blood tests help determine severity. Raised white cell count and CRP suggest inflammation. Abnormal liver enzymes may indicate bile duct obstruction or pancreatitis.
Understanding these basics helps patients follow clinical discussions and understand why recommendations may change after test results.
Laparoscopic Cholecystectomy Explained
Laparoscopic cholecystectomy is the standard operation for symptomatic gallstones. It is performed under general anaesthetic using small incisions and a camera.
The gallbladder is separated from the liver and removed through a small port. Most procedures last under an hour.
Benefits of Keyhole Surgery
- Smaller scars
- Reduced postoperative pain
- Short hospital stay
- Faster return to normal activity
Conversion to open surgery is uncommon but may be required for safety in complex cases.
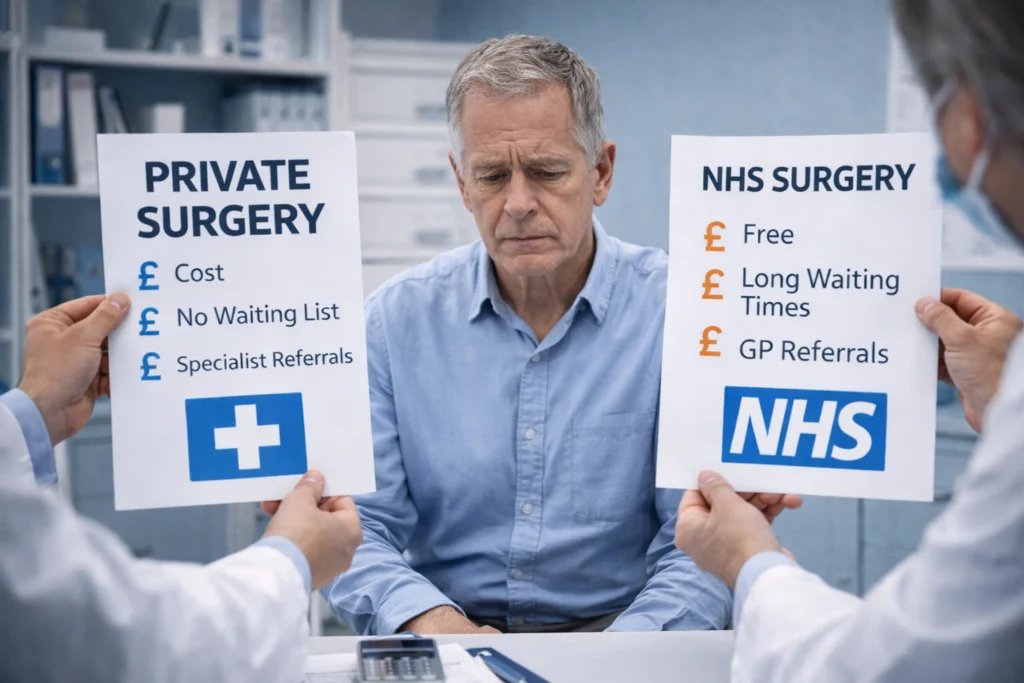
NHS vs Private Treatment Pathways in the UK
NHS Pathway
Patients are usually referred by their GP for ultrasound and surgical assessment. Waiting times vary by region and urgency. Emergency cases are prioritised, while elective surgery may involve longer waits.
Private Pathway
Private care often offers quicker access to imaging, consultation, and surgery scheduling. The surgical technique and safety standards are equivalent, but timelines and continuity of care differ.
Choosing between pathways depends on symptom burden, work commitments, and personal circumstances.
Recovery Timelines After Gallbladder Surgery
Most patients are discharged the same day or after one night in hospital.
Typical Recovery Milestones
- Light activity: within a few days
- Desk-based work: 1–2 weeks
- Driving: around 1 week if pain-free
- Full activity: 4–6 weeks
Digestive changes such as loose stools or bloating may occur initially but usually settle within weeks.
Risks and Complications to Be Aware Of
Laparoscopic cholecystectomy is very safe. However, potential risks include bleeding, infection, bile leak, and bile duct injury. These complications are uncommon and are carefully monitored for.
Understanding risks supports informed decision-making and realistic expectations.
The Takeaway
Gallbladder pain should not be ignored, but surgery is not always urgent or inevitable. The right decision depends on symptoms, imaging findings, and risk of complications. A good surgeon acts as a guide, helping you choose the safest option at the right time.
Frequently Asked Questions
Gallbladder pain can settle temporarily, especially if attacks are mild and diet-related. However, gallstones usually remain, and many patients experience repeat episodes over time. Symptoms should be monitored rather than ignored.
No. Gallstones that cause no symptoms often need no treatment. Surgery is usually recommended only when gallstones cause pain, inflammation, or complications such as infection or pancreatitis.
Pain lasting longer than six hours, pain with fever, jaundice, vomiting, or worsening symptoms should be assessed urgently. These signs may indicate gallbladder inflammation or bile duct blockage.
Ultrasound is the main test used to identify gallstones and gallbladder inflammation. Blood tests help detect infection, inflammation, and bile duct involvement. Additional scans are only needed in selected cases.
It is a routine but significant operation performed under general anaesthetic. Recovery is usually quicker than open surgery, and most patients go home the same day or after one night.
In many cases, yes. Repeated inflammation can make surgery more complex. Planned surgery often leads to smoother recovery compared to emergency procedures.